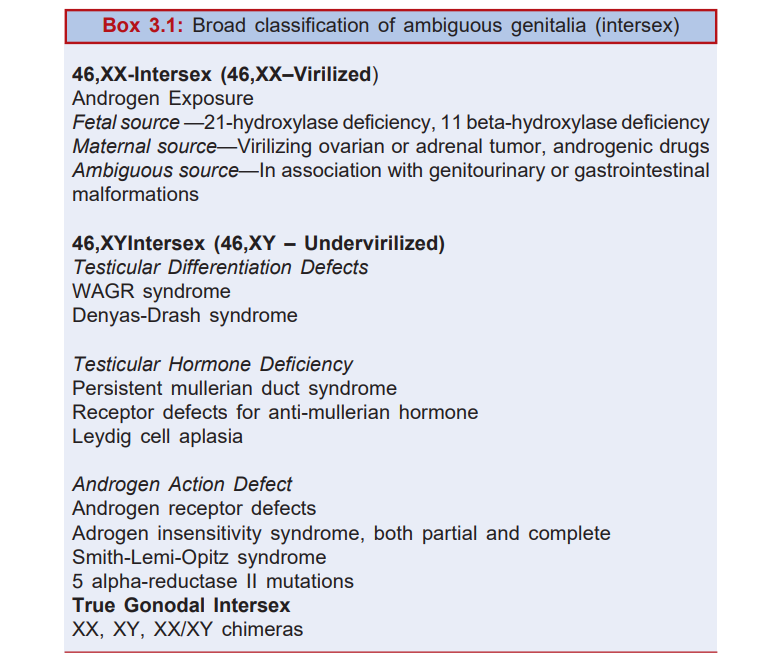
The term, ambiguous genitalia, denotes discrepancy between the actual sex and the bizarre external genitalia (Box 3.1). The latter are characteristic of neither a male nor a female. The entity is also called hermaphroditism (herm referring to “good” and aphroditism to “goddess”). Ambiguity results from excessive virilization of a female (female hermaphroditism) or defect in masculinization of a male (male hermaphroditism). Hermaphroditism must be suspected in any male child with a small penis, hypospadias and undescended testes. Any girl with a doubtful mass in the labia majora or groin needs to be examined to a certain if the mass could be testes. The history should trace the presence of intersex siblings or such other close relatives and the mode of inheritance. A history of consanguinity is of vital importance. Was the mother on hormonal therapy during the pregnancy? What was the time sequence of appearance of secondary sex characters in the child with ambiguous sex problem? The physical examination should confirm the presence or absence of testes (in the scrotum or inguinal canal), the degree of labioscrotal fusion, size of penis or clitoris, hypospadias, and uterus through rectal examination. Search should also be made for renal, anal and other congenital anomalies. Presence of two labioscrotal masses confirms the existence of two testes. Possibility of female pseudohermaphroditism is thereby immediately rule out. Investigations include buccal smear to know the real gonadal sex (negative in male hermaphroditism and positive in true
Differential Diagnosis in Pediatrics
hermaphroditism and female pseudohermaphroditism), 17-ketosteroids and pregnantriol in urine, serum electrolytes, chromosomal studies and X-ray studies. Gonadal biopsy is a must when gonads are in the abdomen and in certain other vague cases. In many instances, laparotomy may be warranted to be certain of the diagnosis.
True Hermaphroditism
This condition is quite rare. A sheer over 500 cases are on record. In this state, both ovarian and testicular tissues are present either in the same or in the opposite gonads. The external genitalia are usually ambiguous. The pheno-type may, however, be male or female. Ovotestis is the most frequently seen gonad in true hermaphroditism. The testicular tissue in such an ovotestis is, however, defective. As a result, secretion of androgens and antimullerian hormone is grossly inadequate. A true hermaphrodite is best brought up as a female with selective removal of testicular tissue.
Male Pseudohermaphroditism
This condition is generally characterized by male phenotype. The penis is small with hypospadias (Fig. 3.1). Testes are undescended. Labioscrotal folds are fused. A casual look gives an impression of female genitalia. The genotype is XY. Incomplete virilization of the external genitalia is the main problem. Its causes include defects intesticular differentiation (Camptomelic syndrome), pure gonadal dysgenesis (Swear syndrome), gonadal agenesis (embryonic testicular regression syndrome), and defects in

Fig. 3.1: Male pseudohermaphroditism Note that the external genitalia are confusing. Whether the child has a small penis with hypospadias or it is indeed a virilized clitoris is apparently not clear. What indeed clinched the diagnosis in this child was palpability of two testes in the so-called “labioscrotal” sac. Gonadal biopsy showed purely testicular tissue that was dysgenetic.
testicular hormones (uterine hernia syndrome), and defects in androgen action (5 alpha-reductase deficiency, testicular feminization syndrome, Reifenstein syndrome.
Female Pseudohermaphroditism
This is the most common type of hermaphroditism. It is characterized by masculinization of the genetically female child. Ovaries are present. Clitoris is large enough and looks like penis. Labia majora is large and may be fused, giving the appearance of a scrotal sac. Its causes include excessive intake of androgens by the mother, congenital adrenal hyperplasia and maternal virilizing tumors. Congenital adrenal hyperplasia is by and large the most common cause of female hermaphroditism. Masculinization may be to the extent of development of a false penile urethra. The child looks a male with cryptorchidism. Degree of virilization is greater in salt-losers than non-salt-losers. It is highest with 21-hydroxylase and 11- hydroxylase defects
FURTHER READING
- Rapaport R. Intersex. In: Kliegman RM, Behrman RE, Jenson HB, Stanton BL (Eds): Nelson Textbook of Pediatrics,18th edn. Philadelphia: Saunders 2008:2394-2403.
- White PC, Speicer PW. Congenital adrenal hyperplasia due to 21- hydroxylase deficiency. Endoc Rev 2000;21:245-249.
RELATED POST

Empyema Thoracis

Bell Palsy (Peripheral Facial Palsy)

Opportunistic Infections