Floppy baby syndrome refers to an infant’s flabby muscles. This symptom complex might mask a variety of illnesses, ranging from benign congenital hypotonia to Down syndrome and Werdnig-Hoffmann disease.
The interrogation must determine if the floppiness has been present since birth or developed later. Is it staying the same, getting better, or becoming worse? Is there a problem with eating, breathing, lethargy, hoarseness, physiologic icterus prolongation, or anemia that isn’t responding to standard treatment? Is there any mental or developmental impairment? Is there any previous history of birth trauma or asphyxia? Have you had any seizures? Is there any evidence of a previous illness? Is there a sibling or family member who has had a similar illness? Is there a lack of or a decline in fetal movements in the mother’s womb? Is it possible that she has myasthenia gravis?
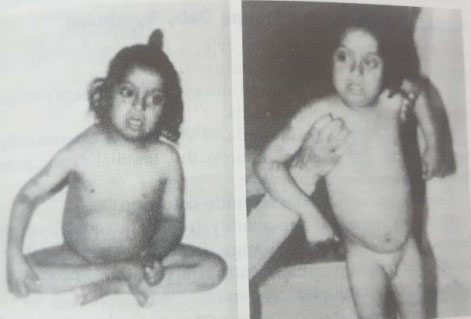
First and foremost, a physical examination must be conducted to determine whether the child is actually floppy, with notable hypotonia in all of his muscles, particularly the skeletal muscles. Hypotonia is best understood by observations of ventral suspension (Figs 26.1 and 26.2) and “pull-to-sit.” What is the current situation with tendon reflexes? Is there any sensory input? Is there any mental or developmental disability, and how severe is it? Is there any engagement of the tongue, jaw, or facial muscles? Is there any protection for extraocular muscles or sphincters? Is there any involvement of the respiratory muscles? Are there any facial characteristics that are linked to Down syndrome or cretinism? Is he overweight? Is he severely undernourished? Is there any sign of rickets or scurvy?
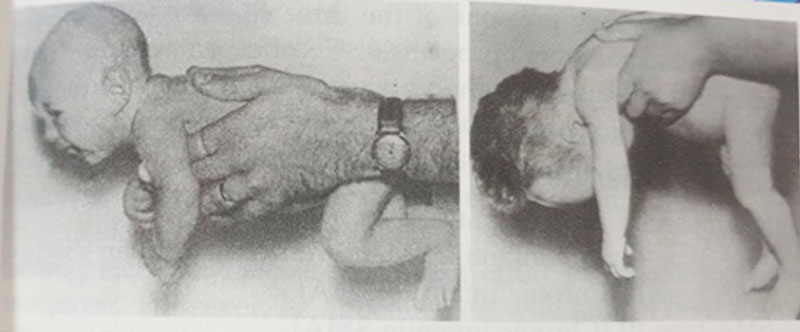
Figs 26.1 and 26.2: Floppy baby. On ventral suspension (Fig. 26.2), observe the considerable hypotonia (weakness) of the limbs, trunk, and neck, as well as the usual reaction in a healthy child (Fig. 26.1).

Fig. 26.3: Spinal muscular atrophy (SMA) type 1 (Werdnig-Hoffmann disease). Note the frog-leg position of the lower limbs, as well as the external rotation of the shoulders and chest retraction.
Benign Congenital Hypotonia
The appearance of gross hypotonia and delayed motor development define this disorder, which can be hereditary in some cases. The muscles of the baby are soft and flabby, allowing for a wide range of motion. Some tendon reflexes can be elicited, whereas others cannot. There are a lot of spontaneous motions. It is common for individuals to grow intellectually.
The condition might progress in one of three ways. First, it may stay non-progressive and stagnant. Second, some children acquire contractures, despite the fact that their joints are constantly hypermobile. Third, by the age of 8 to 10 years, the majority of individuals have entirely recovered.
Spinal Muscular Atrophy
Spinal muscular atrophy may be of four types:
SMA type I (acute infantile SMA, Werdnig Hoffman disease)
SMA type II (Chronic infantile SMA)
SMA type III (Chronic juvenile SMA)
SMA type IV (adult SMA)
Werdnig-Hoffmann disease, commonly known as spinal muscular atrophy (type I), is an autosomal recessive ailment marked by positive family history, the lack or decrease of fetal movements in gestation, and symptoms emerging before the age of two years, and, in many cases, directly before birth.
Gross hypotonia with areflexia is a condition that often appears in infancy. With abduction at the hips and flexion at the knees, the legs acquire the so-called “frog leg position.” The intercostal and bulbar muscles are implicated, but the diaphragm is mostly unaffected, culminating in paradoxical breathing with inside chest movement on inhalation. In the tongue, fasciculations or fibrillations can be seen, as well as atrophy. On the other hand, mental growth is extremely typical. In the beginning, the newborn is likely to be overweight.
The condition advances fast in the vast majority of instances, eventually killing the child. Neurologic involvement of the thoracic muscles, respiratory failure, food aspiration, and/or fulminant illness are the causes of mortality. Survivors seldom reach puberty, and even fewer reach maturity, and they are absolutely incapable.
The majority of the time, the diagnosis is clinical. Muscular biopsy reveals classic denervation atrophy characteristics, such as vast regions of tiny atrophic fibers and remnant muscle fibers with or slightly increased diameter.
Myasthenia Gravis
This condition, which is caused by an immunological response to cholinergic receptors, is thought to be the cause of infant floppiness. There are two distinct types:
The first form is transient neonatal myasthenia gravis, which occurs when a child inherits myasthenia gravis from a mother who has an established, mild, or perhaps undiagnosed condition. With inadequate feeding, a weak cry, a weak respiratory effort, a lot of oral secretions, and ptosis, the newborn is considered as floppy and weak. He seems awake, nevertheless, with typical deep tendon reflexes. The intramuscular administration of edrophonium/neostigmine produces outstanding results. Many infants heal on their own within 3 to 4 weeks, even without any treatment.
The second kind, persistent newborn myasthenia gravis, occurs when the mother has no signs or symptoms of the condition. The likelihood of the illness affecting additional siblings is high. The eyelids and extraocular muscles are significantly damaged, in addition to indications of the transitory type. It is likely to last for the rest of one’s life.
Cerebral Palsy
Floppiness is associated with two types of non progressive central motor deficits that occur during the prenatal, natal, or postpartum period (most often cerebral anoxia).
Hypotonia, motor impairment, and severe mental retardation are all symptoms of atonic diplegia. Tendon reflexes are simple to induce. These might be rather quick. Spasticity occurs in the youngster as he or she grows older.
Hypotonia, hypoactive tendon reflexes, and later gait ataxia with intention tremors are all symptoms of congenital cerebellar ataxia, a rare type of cerebral palsy. There is a chance that mild mental impairment and nystagmus may occur.
Congenital Hypothyroidism
Hypotonia, lethargy, sluggishness, hoarse scream, feeding trouble, oversleeping, chronic jaundice, persistent constipation, abdominal distention with umbilical hernia, cold, rough, dry and thickened skin, a thickened projecting tongue, a very big posterior fontanel, and anemia that responds poorly to hematinics are all symptoms of hypothyroidism in the newborn. When the baby is born, he or she is generally big and weighty.
It takes a few weeks (8 to 12) for the characteristic traits of certainism to manifest (Fig. 26.4). A huge tongue protrudes from a large open mouth with thick lips, puffy eyelids, depressed nasal bridge, pseudohypertelorism, wrinkled forehead with sparse brows, and hairline reaching extremely low fat. Hair on the scalp is sparse, scratchy, dry, and fragile. It has a tough, thick layer of skin on top of it. The neck is short, and a dry, chilly supraclavicular pad is frequently present. Sutures in the anterior fontanel and coronal regions are frequently wide open. The sound of voice becomes hoarse. The development of the dentition is delayed. It is almost as though floppiness is the rule. The abdomen is frequently enlarged, and there is an umbilical hernia of varying size. The fingers are short and the hands are wide. Constipation is common, and it does not react to laxatives or changes in feeding schedules.
Mental retardation, as well as physical and growth retardation, are generally seen together. The ratio of upper to lower parts may remain infantile, i.e., 1.7:1.
X-ray scans for bone age and epiphyseal dysgenesis, raised blood cholesterol, low serum alkaline phosphatase, low PBI, low radioactive iodine (131I), high plasma TSH3, and, most significantly, low T3 and T4 may all be used to confirm the diagnosis.

Fig. 26.4: Congenital hypothyroidism. This intellectually and physically impaired youngster has infantile body proportions and typical coarse face characteristics, as well as a short neck.
Down Syndrome
Because of the characteristic stigmata, such as visible features and mental retardation, it is not difficult to diagnose Down syndrome, the 21 trisomy, in a floppy newborn, similar to congenital hypothyroidism.
The baby has microcephaly, a low hairline, and a small neck, thus he’s apparently a cheerful idiot (Figs 26.5 and 26.6). The upward slant of the eyes, epicanthal wrinkles, and Brushfield patches are all common facial traits. The nose is small, with a flattened bridge that, when combined with epicanthal folds, provides the appearance of increased distance between the eyes, a condition known as “pseudohypertelorism.” The so-called “scrotal tongue” protrudes from a tiny buccal cavity and may be furrowed. Low-set ears that may be malformed. There may be a high-arched palate and malocclusion of the teeth.Because of the rudimentary middle phalanx, the hands are short and wide, with a single palmar wrinkle (Simian crease) and an in-bent little finger. The big and second toes have a large space between them, and there is sometimes a deep furrow between them and the sole.
Figs 26.5 and 26.6:Down syndrome.Note the upturned eyes, epicanthal folds, depressed bridge of the nose, widely separated eyes, and short neck and hypotonia. The IQ was only 30. He also has a bent little finger, VSD, and a Simian crease (bilateral) (bilateral).
Congenital cardiac disease, duodenal atresia, Hirschsprung disease, and leukemia are all much more common in people with Down syndrome.
Prader-Willi Syndrome
Prader-Willi syndrome is characterized by a high level of floppiness. Obesity, hypotonia, hypogonadism, strabismus, and a propensity to diabetes mellitus are the main symptoms of the syndrome.
Marfan Syndrome
Muscle floppiness, arachnodactyly (spider fingers), and hyperextensibility of the joints may be seen in this congenital connective tissue condition in the newborn and early infancy. Early in childhood, lenticular subluxation and aortic dilatation might occur.
Drugs
Diazepam, tricyclic antidepressants, kanamycin, colistin sulfalc,cycloserine, ethionamide, gentamicin, nitrofurantoin, neomycin, INH, cyclophosphamide, 6-MP, meprobomate, lead, vincristine.
Remaining Causes of Floppy Baby Syndrome
CNS Kernicterus, chromosomal abnormalities, Lowe (oculocerebrorenal) syndrome, cerebral lipidosis, and mucoviscidosis are some of the conditions that might cause the floppy baby syndrome.
Spinal cord: Trauma, epidural abscess, shock phase of transverse myelitis, and severe poliomyelitis all affect the spinal cord.
Peripheral nerves: Guillain-Barré syndrome, severe diphtheritic paralysis, arsenical neuropathy, familial dysautonomia, and congenital sensory neuropathy are all examples of peripheral nerve disorders.
Neuromuscular junction: Botulism in children.
Muscles: Congenital muscular dystrophy, myotonic dystrophy, Pompe type glycogen storage disease, central core disease, nemaline myopathy, mitochondrial myopathies, polymyositis arthrogryposis multiplex congenita are all muscle disorders.
Miscellaneous: Advanced protein-energy malnutrition, rickets, scurvy, acrodynia, Ehler-Danlos syndrome, cutis laxa, and other conditions.
RELATED POST

Empyema Thoracis

Bell Palsy (Peripheral Facial Palsy)

Opportunistic Infections